Naseer Ahmad
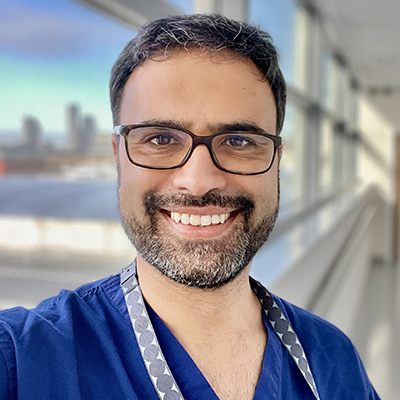
Naseer is a vascular surgeon based at Manchester University Foundation Trust. He performs the full range of vascular procedures including carotid, aneurysm and venous surgery but specialises in complex lower limb surgery that prevents an amputation.
He is the Clinical Director of both the Manchester Amputation Reduction Strategy (The MARS Project) and the Greater Manchester & East Cheshire Aneurysm Screening Programme and the former Deputy Chief Clinical Information Officer of his hospital.
His award winning research interest is the inequality surrounding lower limb amputations which led to developing The MARS Project. This project has resulted in a 46% reduction in amputation prevalence over 6 years in a pilot site of 220 000 people. This work is currently being scaled up for 3 million people. His cross-sectoral roles are now enabling him to develop ‘whole systems’ pathways i.e. those that harmonise Public Health, community and hospital services for patients with vascular disease.
His aim is to bring together and digitise siloed NHS services and is working with leaders across Manchester’s academic, clinical, strategic, financial and digital areas to drive this forward.
Presentation at The Society of Tissue Viability 2025 Conference
Understanding how to navigate the system and implement change (including cultural change)
JOINT PRESENTATION WITH DR KRISTEN SORENSEN
Key messages
-
Planning is key: Invest time in co-designing and planning what “good” looks like, ensuring alignment with wider health priorities and system goals. Be inclusive.
-
Collaborative leadership drives change: Build strong relationships across stakeholders, including Public Health, hospitals, community services, commissioners, academia, and strategic networks. Be collaborative.
-
Focus on sustainable, evidence-based care: Elevate care standards (e.g., diabetes multidisciplinary team standard) across pathways without compromising existing services. Be evidence based.
-
Streamline for efficiency: Simplify patient pathways, reduce duplication, and address barriers to implementation for cost-effective and impactful results. Be attentive.
-
Think slow, act fast: Thorough preparation allows for rapid, system-wide implementation that transforms outcomes and delivers measurable improvements. Be ready.
Abstract
Background: The Manchester Amputation Reduction Strategy (MARS) has demonstrated remarkable success, reducing lower limb amputations by 46% over six years (2015/16–2021/22) in its pilot area of 210,000 people. This achievement, implemented within existing resources, resulted in annual savings exceeding £200,000 in hospital admission costs alone. Recognised for its impact, MARS is now scaling to serve a population of over 3 million and forms a key component of the Greater Manchester Integrated Care Board’s (ICB) five-year plan.
Methods: The strategy applied Implementation Science principles, emphasising co-design and building collaborative leadership to ensure sustainable practice change. Central to its approach was the clinical principle of elevating lower limb wound care to the diabetes multidisciplinary team standard—without compromising diabetes care. Patient pathways were overhauled to eliminate duplication and improve efficiency. Key to success was fostering collaboration, identifying and addressing barriers, and aligning with system-wide priorities.
Findings: Through careful planning and collaboration, MARS achieved systemic change while saving lives, improving patient outcomes, and reducing healthcare costs. By involving stakeholders across Public Health, community, hospital, digital, commissioning, academia, and the Strategic Clinical Network, the project created a shared vision and actionable plan for reducing amputations.
Key Messages: “Think slow and act fast.” Effective change begins with thorough planning. Engage stakeholders early, build relationships, and align goals with wider health priorities especially those highlighted in the recent Darzi report. By speaking the system’s language and understanding its complexities, sustainable, impactful change can be delivered swiftly and effectively. MARS is proof that integrated care, collaboration, and evidence-based practice can transform outcomes.
Presentation at The SoTV/EWMA 2024 Conference, London
How Greater Manchester made wound care a system wide priority in their 5 year plan
Objectives
After attending this session, persons will be able to:
- To understand implementation process models and theoretical frameworks
- To understand barriers and facilitators to implementing integrated leg ulcer pathways, vascular assessment training and vascular assessment quality improvement initiatives in Greater Manchester
Abstract
Greater Manchester ICB has made wound care part of its’ 5 year strategy. This was developed using data provided by The Manchester Amputation Reduction Strategy (MARS).
We delivered a 42% reduction in amputation number over a six year period in our pilot area of 220 000. We advanced a ‘whole systems’ approach routed in reducing inequality and allowing all lower limb wounds the same multi-disciplinary care enjoyed by diabetic foot ulcer patients.
We created capacity, within existing resource, through co-designing change and integrated working across podiatry, nursing teams and vascular teams facilitated by the harmonisation of pathways and culture.
We built lasting relationships across traditionally siloed teams and upskilled wider team members to order duplex, CT and MR scans. We are now scaling up this work across the region.














